Swiss Policy Research
On the development of the pandemic
In most Western countries, the peak of coronavirus infections was already reached in March or April and often before the lockdown. The peak of deaths in most Western countries was in April. Since then, hospitalizations and deaths have been declining in most Western countries (see graphs below).
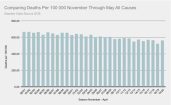
This development also applies to countries without a lockdown, such as Sweden, Belarus and Japan. Cumulative annual mortality in most western countries continues to be in the range of a mild (e.g. CH, AT, DE) to strong (e.g. USA, UK) influenza season.
After the end of the lockdowns, the number of corona tests in the low-risk general population has increased strongly in many countries, for example in connection with people returning to work and school.
This led to a certain increase in positive test results in some countries or regions, which was portrayed by many media and authorities as an allegedly dangerous increase in “case numbers” and sometimes led to new restrictions, even if the rate of positive tests remained very low.
“Case numbers” are, however, a misleading figure that cannot be equated with sick or infected people. A positive test can, for example, be due to non-infectious virus fragments, an asymptomatic infection, a repeated test, or a false-positive result.
Moreover, counting alleged “case numbers” is not meaningful simply because antibody tests and immunological tests have long shown that the new coronavirus is up to fifty times more widespread than assumed on the basis of daily PCR tests.
Rather, the decisive figures are the number of sick people, hospitalisations and deaths. It should be noted, however, that many hospitals are now back to normal operation and all patients, including asymptomatic patients, are additionally tested for the coronavirus. Therefore, what matters is the number of actual Covid patients in hospitals and ICUs.
In the case of Sweden, for example, the WHO had to withdraw the classification as a “risk country” after it became clear that the apparent increase in “cases” was due to an increase in testing. In fact, hospitalisations and deaths in Sweden have been declining since April.
Some countries have already been in a state of below-average mortalitysince May. The reason for this is that the median age of corona deaths was often higher than the average life expectancy, as up to 80% of deathsoccurred in nursing homes.
In countries and regions where the spread of the coronavirus has so far been greatly reduced, it is nevertheless entirely possible that there will be a renewed increase in Covid patients. In these cases, early and effective treatment is important (see below).
Global Covid-19 mortality is currently – despite the significantly older population nowadays – a whole order of magnitude below the flu pandemics of 1957 (Asian flu) and 1968 (Hong Kong flu) and in the range ofthe rather mild “swine flu pandemic” of 2009.
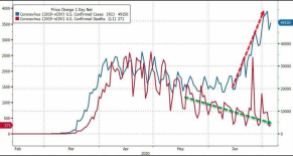
The following charts illustrate the discrepancy between “cases”, patients and deaths.
Charts: “Cases”, deaths, and mortality in different countries
On the lethality of Covid-19
Most antibody studies have shown a population-based Infection Fatality Rate (IFR) of 0.1% to 0.3%. The US health authority CDC published in May a still cautious “best estimate” of 0.26% (based on 35% asymptomatic cases).
At the end of May, however, an immunological study by the University of Zurich was published, which for the first time showed that the usual antibody tests that measure antibodies in the blood (IgG and IgM) can detect at most about one fifth of all coronavirus infections.
The reason for this is that in most people the new coronavirus is already neutralised by antibodies on the mucous membrane (IgA) or by cellular immunity (T cells) and no symptoms or only mild symptoms develop.
This means that the new coronavirus is probably much more widespread than previously assumed and the lethality per infection is around five times lower than previously estimated. The real lethality could therefore be significantly below 0.1% and thus in the range of influenza.
At the same time, the Swiss study may explain why children usually develop no symptoms (due to frequent contact with previous corona cold viruses), and why even hotspots such as New York City found an antibody prevalence (IgG/IgM) of at most 20% – as this already corresponds to herd immunity.
The Swiss study has in the meantime been confirmed by several more studies:
- A Swedish study showed that people with mild or asymptomatic disease often neutralized the virus with T-cells without the need to produce antibodies. Overall, T-cell immunity was about twice as common as antibody immunity.
- A large Spanish antibody study published in Lancet showed that less than 20% of symptomatic people and about 2% of asymptomatic people had IgG antibodies.
- A German study (preprint) showed that 81% of the people who had not yet had contact with the new corona virus already had cross-reactive T-cells and thus a certain background immunity (due to contact with previous corona cold viruses).
- A Chinese study in the journal Nature showed that in 40% of asymptomatic persons and in 12.9% of symptomatic persons no IgG antibodies are detectable after the recovery phase.
- Another Chinese study with almost 25,000 clinic employees in Wuhan showed that at most one fifth of the presumably infected employees had IgG antibodies (press article).
- A small French study (preprint) showed that six of eight infected family members of Covid patients developed a temporary T-cell immunity without antibodies.
Video interview: Swedish Doctor: T-cell immunity and the truth about Covid-19 in Sweden
In this context, a US study in the journal Science Translational Medicine, using various indicators, concluded that the lethality of Covid-19 was much lower than originally assumed, but that its spread in some hotspots was up to 80 times faster than suspected, which would explain the rapid but short-duration increase in patients.
A study in the Austrian ski resort of Ischgl, one of the first European “corona hotspots”, found antibodies in 42% of the population. 85% of the infections went “unnoticed” (i.e. very mild), about 50% of the infections went completely without (noticeable) symptoms.
The high antibody value of 42% in Ischgl was due to the fact that Ischgl also tested for IgA antibodies in the blood (instead of only IgM/IgG). Additional tests for mucosal IgA and for T-cells would undoubtedly have shown even higher immunity levels close to herd immunity.
With only two deaths (both of them men over 80 years of age with preconditions), the population-based covid lethality (IFR) in the “hotspot” Ischgl is significantly below 0.1%.
Due to its rather low lethality, Covid-19 falls at most into level 2 of the five-level pandemic plan developed by US health authorities. For this level, only the “voluntary isolation of sick people” is to be applied, while further measures such as face masks, school closings, distance rules, contact tracing, vaccinations and lockdowns of entire societies are not recommended.
The new immunological results also mean that “immunity passports” and mass vaccinations are unlikely to work and are therefore not a useful strategy.
Some media continue to speak of allegedly much higher Covid lethality levels. However, these media refer to outdated simulation models, confuse mortality and lethality, or CFR and IFR, or “raw IFR” and population-based IFR. More about these errors here.
In July, an antibody prevalence of allegedly up to 70% was reported in some New York City districts. However, this is not a population-based figure, but rather antibodies in people who had visited an urgent care center.
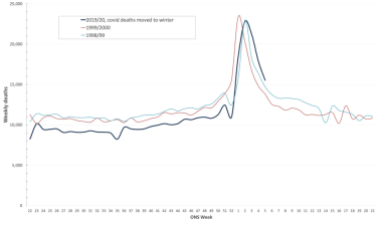
The following graph shows the actual development of corona deaths in Sweden (no lockdown, no face mask obligation) compared to the forecasts of Imperial College London (orange: no measures; grey: moderate measures). Swedish annual all-cause mortality actually is in the range of a medium flu wave and 3.6% lower than in previous years.
 Corona deaths in Sweden: ICL prediction versus reality (HTY/FOHM)
Corona deaths in Sweden: ICL prediction versus reality (HTY/FOHM)
On the health risks of Covid-19
Why is the new coronavirus harmless for many people, but very dangerous for some people? The reason has to to with special features of the virus and the human immune system.
Many people, including almost all children, can neutralise the new corona virus with an existing immunity (due to contact with previous corona cold viruses) or through antibodies on the mucous membranes (IgA), without it causing much damage.
However, if this does not succeed, the virus can penetrate the organism. There the virus can cause complications in the lung (pneumonia), the blood vessels (thromboses, embolisms), and other organs due to its efficient use of the human ACE2 cell receptor.
If in this case the immune system reacts too weakly (in older people) or too strongly (in some younger people), the course of the disease can become critical.
It has also been confirmed that the symptoms or complications of serious Covid-19 disease can last for weeks or even months in some cases.
Therefore, the new coronavirus should not be underestimated and earlyand effective treatment is absolutely crucial for patients at risk.
In the longer term, the new coronavirus could develop into a typical cold virus, similar to the coronavirus NL63, which also uses the ACE2 cell receptor and nowadays affects primarily young children and nursing patients, causing upper and lower respiratory tract infections.
On the treatment of Covid-19
Note: Patients are asked to consult a doctor.
Several studies have now confirmed what some front-line physicians have been saying since March: Early treatment of Covid patients with zinc and the malaria drug hydroxychloroquine (HCQ) is indeed effective. US doctors have reported a reduction in hospitalisation rates of up to 84% and a stabilisation of the health condition often within a few hours.
Zinc has antiviral properties, HCQ supports zinc absorption and has additional antiviral properties. These drugs are supplemented by doctors if necessary with an antibiotic (to prevent a bacterial superinfection) and a blood thinner (to prevent infection-related thromboses and embolisms).
The alleged or actual negative results with HCQ in some studies were based, according to the current state of knowledge, on delayed use(intensive care patients), excessive doses (up to 2400mg per day), manipulated data sets, or ignored contraindications (e.g., favism or heart problems).
Sadly, the WHO, many media and some authorities may have caused considerable and unnecessary damage to public health in recent months through their negative stance, which may have been politically motivated or influenced by pharmaceutical interests.
French professor of medicine Jaouad Zemmouri, for example, estimates that Europe could have avoided up to 78% of Covid deaths by adopting a consistent HCQ treatment strategy.
HCQ contraindications such as favism or heart problems need to be considered, but the recent Ford Medical Center study achieved a reduction in hospital deaths of around 50% even with 56% African-American patients (who more often have favism).
However, the crucial point in the treatment of high-risk patients is early intervention as soon as the first typical symptoms develop and even without a PCR test in order to prevent progression of the disease and avoid intensive care hospitalization.
Most countries did the exact opposite: after the infection wave in March, they imposed a lockdown, so that infected and frightened people were locked up in their homes without treatment and often waited until they developed severe respiratory distress and had to be taken directly to the intensive care unit, where they were often sedated and intubated and were likely to die.
It is conceivable that a zinc HCQ combination protocol, which is simple, safe and inexpensive, could make more complex drugs, vaccinations and measures largely obsolete.
More recently, a case study from France showed that in four of the first five patients treated with the much more expensive drug Remdesivir from the pharmaceutical company Gilead, treatment had to be discontinued due to liver issues and kidney failure.
Read more: On the treatment of Covid-19
On the effectiveness of masks
Various countries have introduced or are currently discussing the introduction of mandatory masks in public transport, in shopping malls, or generally in public.
Due to the lower-than-expected lethality of Covid-19 and the available treatment options, this discussion might become obsolete. The original argument regarding a reduction of hospitalizations (“flatten the curve”) is also no longer relevant, as the hospitalization rate was and is about twenty times lower than initially assumed.
Nevertheless, the question of the effectiveness of masks can be asked. In the case of influenza epidemics, the answer is already clear from a scientific point of view: masks in everyday life have no or very little effect. If used improperly, they can even increase the risk of infection.
Ironically, the best and most recent example of this is the often-mentioned Japan: Despite its ubiquitous masks, Japan experienced its most recent strong flu wave – with around five million people falling ill – just one year ago, in January and February 2019.
However, unlike SARS corona viruses, influenza viruses are transmitted also by children. Indeed, Japan had to close around ten thousand schools in 2019 due to acute outbreaks of the flu.
With the SARS 1 virus of 2002 and 2003, there is some evidence that medicalmasks can provide partial protection against infection. But SARS-1 spread almost exclusively in hospitals, i.e. in a professional environment, and hardly to the general public at large.
In contrast, a study from 2015 showed that the cloth masks in use today are permeable to 97% of viral particles due to their pore size and can further increase the risk of infection by storing moisture.
Some studies recently argued that everyday masks are nevertheless effective in the case of the new coronavirus and could at least prevent the infection of other people. However, these studies suffer from poor methodology and sometimes show the opposite of what they claim.
Typically, these studies ignore the effect of other simultaneous measures, the natural development of infection numbers, changes in test activity, or they compare countries with very different conditions.
An overview:
- A German study claimed that the introduction of compulsory masks in German cities had led to a decrease in infections. But the data does not support this: in some cities there was no change, in others a decrease, in others an increase in infections (see graph below). The city of Jena, presented as a model, simultaneously introduced the strictest quarantine rules in Germany, but the study did not mention this.
- A study in the journal PNAS claimed that masks had led to a decrease in infections in three hotspots (including New York City). This did not take into account the natural decrease in infections and other measures. The study was so flawed that over 40 scientists recommended that the study be withdrawn.
- A US study claimed that compulsory masks had led to a decrease in infections in 15 states. The study did not take into account that the incidence of infection was already declining in most states at that time. A comparison with other states was not made.
- A Canadian study claimed that countries with compulsory masks had fewer deaths than countries without compulsory masks. But the study compared African, Latin American, Asian and Eastern European countries with very different infection rates and population structures.
- A meta-study in the journal Lancet claimed that masks “could” lead to a reduction in the risk of infection, but the studies considered mainly hospitals (Sars-1) and the strength of the evidence was reported as “low”.
The medical benefit of compulsory masks therefore continues to remain questionable. In any case, a comparative study by the University of East Anglia came to the conclusion that compulsory masks had no measurable effect on the incidence of Covid infections or deaths.
It is also clear that widespread face masks couldn’t stop the initial outbreak in Wuhan.
Sweden showed that even without a lockdown, without compulsory masks and with one of the lowest intensive care bed capacities in Europe, hospitals need not be overburdened. In fact, Sweden’s annual all-cause mortality is in the range of previous flu seasons.
At any rate, authorities shouldn’t suggest to the population that compulsory masks reduce the risk of infection, for example in public transport, as there is no evidence of this. Whether with or without masks, there is an increased risk of infection in densely packed indoor areas.
Interestingly, the demand for a worldwide obligation to wear masks is led by a lobby group called “masks4all” (masks for all), which was founded by a “young leader” of the Davos forum.
 Mandatory masks in German cities: no relevant impact. (IZA 2020)
Mandatory masks in German cities: no relevant impact. (IZA 2020)
The role of contact tracing
Numerous countries have introduced smartphone apps and special units for “contact tracing”. However, there is no evidence that these can make an epidemiologically relevant contribution.
In the case of tracing pioneer Iceland, the app has largely failed, in Norway it was stopped for data protection reasons, in India, Argentina, Singapore and other countries it became mandatory after all, in Israel contact tracing is operated directly by the secret service.
A WHO study on influenza pandemics in 2019 came to the conclusion that contact tracing is not useful from an epidemiological point of view and “is not recommended in any circumstances”. The typical area of application is rather sexually transmitted diseases or food poisoning.
Moreover, serious concerns about data protection and civil rights remain.
NSA whistleblower Edward Snowden warned as early as March that governments could use the corona crisis as an occasion or pretext for expanding global surveillance and control, thus creating an “architecture of oppression”.
A whistleblower who had taken part in a training program for contact tracers in the US described it as “totalitarian” and a “danger to society”.
Swiss computer science professor Serge Vaudenay showed that the contact tracing protocols are by no means “decentralized” and “transparent”, because the actual functionality is implemented through a Google and Apple interface (GAEN) that is not “open source”.
This interface has now been integrated by Google and Apple into three billion mobile phones. According to Prof. Vaudenay, the interface may record and store all contacts, not just those that are medically “relevant”. A German IT expert, for his part, described tracing apps as a “Trojan horse”.
For more information on “contact tracing”, see the June update.
See also: Inside the NSA’s Secret Tool for Mapping Your Social Network(Wired)
 “Contact Tracing” powered by Google und Apple
“Contact Tracing” powered by Google und Apple
On the origin of the new coronavirus
In the June update it was shown that renowned virologists consider a laboratory origin of the new coronavirus to be “at least as plausible” as a natural origin. This is due to some genetic peculiarities of the virus in the area of receptor binding, which lead to particularly high transmissibility and infectivity in humans.
In the meantime, further evidence for this hypothesis has emerged. It was already known that the virus most closely related to SARS-CoV-2 was found in 2013 in southwest China. This bat corona virus was discovered by researchers from the Wuhan Virological Institute and is known as RaTG13.
However, researchers with access to Chinese papers have since found out that the Wuhan scientists did not reveal the whole story. In fact, RaTG13 was found in a former copper mine with a lot of bat feces after six miners fell ill with pneumonia during clean-up work. Three of the miners died.
According to the original Chinese papers, the medical assessment at the time was that these pneumonia cases were caused by a SARS-like virus. But the head of the Wuhan Laboratory strangely said in an interview with the Scientific American in April 2020 that the cause was allegedly a fungus. The institute didn’t disclose that RaTG13 came from that fateful mine, either.
The head of the US “Eco Health Alliance”, which worked together with the Wuhan Institute on virological “gain of function” research (which produces potentially pandemic viruses), claimed that RaTG13 was partially sequenced at the time and then put in a freezer and “not used again until 2020” (when it was compared to SARS-CoV-2).
However, virological database entries found in the meantime show that this is not true either: the virus – then known under the internal code 4991 – was already used for research purposes in the Wuhan laboratory in 2017 and 2018. Moreover, various Chinese virus databases have since been strangely deleted.
Virologists agree that SARS-CoV-2 cannot be a direct, natural successor to RaTG13 – the necessary mutations would take several decades at least, despite a 96 percent genetic match. However, it is theoretically possible that SARS-CoV-2 was generated, based on RaTG13, by virological “gain of function” research in a laboratory, or was itself present in the 2013 mine.
In this sense, it would be conceivable that SARS-CoV-2 could have escaped from the laboratory in Wuhan in September or October 2019 – during a laboratory inspection at that time or during preparations for it. Such laboratory accidents are unfortunately nothing unusual and have already occurred in the past in China, the US, Russia and other countries.
Read more: Seven year coronavirus trail from bat cave via Wuhan lab(Times, July 4, 2020)
Besides the Chinese aspect there is, however, also an American aspect.
It has long been known that US researchers at the University of North Carolina are world leaders in the analysis and synthesis of SARS-like, potentially pandemic viruses. Due to a temporary moratorium in the US, this research was partially transferred to China (i.e. Wuhan) a few years ago.
In April, the Bulgarian investigative journalist Dilyana Gaytandzhieva published information and documents that show that the US Department of Defense, together with the US health authority CDC, was also conducting research on potentially pandemic SARS-like corona viruses.
This corona virus research was carried out in a Pentagon biological laboratory in Georgia (near Russia), among other places, and was also coordinated by the above-mentioned US “Eco Health Alliance”, which cooperated with the Institute of Virology in Wuhan, too. In this respect, the “Eco Health Alliance” may be seen as a military research service provider or contractor.
Thus, apart from its own SARS corona virus research, the US military must have been very familiar with Chinese research in Wuhan, due to its partnership with “Eco Health Alliance”.
Read more: Pentagon biolab discovered MERS and SARS-like coronaviruses in bats (DG)
US investigative journalist Whitney Webb already pointed out that the Johns Hopkins Center for Health Security – which organized the well-known coronavirus pandemic exercise “Event 201” in October 2019 together with the Gates Foundation and the WEF Davos – had also organized the anthrax exercise “Dark Winter” in 2001.
This exercise took place a few months before the actual anthrax attacks in September 2001, whose origin could later be traced back to a Pentagon laboratory. Some of the participants of “Dark Winter” are also involved in the current management of the Corona pandemic.
Developments since the beginning of 2020 show that the new corona virus cannot be seen as a “bioweapon” in the strict sense of the term, as it is not deadly enough and not targeted enough. However, it may well – similar to “terrorists” and amplified by the media – cause fear and terror among the global population and be exploited politically.
In this context, it is noteworthy that vaccine investor and Event 201 cosponsor Bill Gates repeatedly spoke of seeing the current corona virus as “pandemic one”, while “pandemic two” would be a genuine bioterrorist attack for which one must be prepared against.
Nevertheless, besides a potential lab origin, a natural origin continues to be a realistic possibility, even though the “Wuhan wet market” hypothesis and more recently the pangolin hypothesis have already been ruled out by experts.
 Lugar Center: A Pentagon biolab in Georgia that was researching bat coronaviruses (Photo: D. Gaytandzhieva)
Lugar Center: A Pentagon biolab in Georgia that was researching bat coronaviruses (Photo: D. Gaytandzhieva)
(Last updated: July 11)